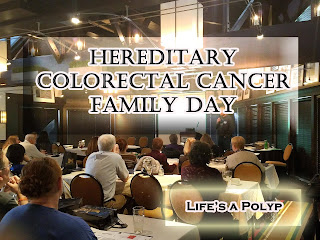
The University of Michigan sponsored a Hereditary Colorectal Cancer Family Day this November in Ann Arbor, Michigan. This wasn't the first year for the family day, but it was my first year to attend. I asked my mother, who also has Familial Polyposis (FAP), to attend with me. Although she was reluctant at first to travel the distance for a two-day trip, she was ultimately glad she attended.
 |
| Me and my mother, Ina. Travis, Carleton, and his son Kevin |
We hopped on a plane on the morning of Friday, November 10 and made our way to Detroit, Michigan where we were warmly greeted by
Kevin, a fellow FAPer and advocate for
FAP and Lynch Peer Support Group in Michigan. That night we were privileged to enjoy a small meet and greet with fellow FAPers - Kevin, his father -
Carleton, and Travis with Hereditary Colon Cancer Foundation.
The following morning the conference started, and we learned about a variety of topics related to Lynch Syndrome and Familial Polyposis. There were an estimated 60 attendees this year - primarily from Michigan. There was a variety of speakers including genetic counselors, doctors of Gastroenterology, Internal Medicine, Surgery, a Dietitian, and Travis.
We learned a great deal of information during this one-day conference. As a child, I had genetic testing completed to confirm my Familial Polyposis suspected diagnosis, but I don't remember ever talking to a genetic counselor afterwards. I visited with one of the genetic counselors to learn more about this area that I hear others talk about frequently. Genetic counselors help individuals gain access to genetic information and technology, genetic testing and diagnosing, and understanding hereditary conditions. They also can help an individual with a hereditary condition obtain testing and counseling for that individual's family members to determine who else in the family may have the condition.
My mother and I weren't very familiar with Lynch Syndrome before this conference. We learned about
Lynch Syndrome from genetic counselors at the University of Michigan Cancer Genetics Department and Dr. C. Richard Boland, himself, who found the gene mutations responsible for Lynch Syndrome. It was interesting to learn that there are 5 different gene mutations that can occur to result in Lynch Syndrome and depending on which gene mutation one has, it will vary the type of cancers the person is predominately at risk for developing. Both syndromes have autosomal dominant inheritance meaning an individual has a 50% chance of inheriting the disease if one of their parents also has the gene.
Lynch Syndrome is also known as Hereditary Non-Polyposis Colon Cancer as the colon isn't carpeted with polyps in the 100s to 1000s as is the case with Familial Polyposis. Although both syndromes have increased risk for other cancers, Lynch has a high occurrence of colorectal cancer, endometrial, and ovarian cancers as well as elevated risk for stomach, liver, urinary tract, central nervous system, small intestine, and sebaceous gland cancers.
FAP on the other hand has elevated risks for cancers of the thyroid, small intestine, liver and smaller but still elevated risks for central nervous system, stomach, pancreas, and bile ducts.
 |
Adenomas (Pre Cancerous Polyps) can look different
|
Screening for cancers is essential for adequate care of Lynch Syndrome and FAP and this includes regular endoscopies and colonoscopies for cancers of the GI tract. Doctors John Carethers, D. Kim Turgeon, and John Byrn explained the colon cancer processes, technology, and techniques used for screening, colonoscopy preps, and surgeries involved for those with both conditions.
Adenomas, precancerous polyps, can vary in shape and size which is why the colonoscopy prep is so important to help the doctor properly identify polyps within the GI tract. There are various prep options including drinks, enemas, meal preps, and pills to help ensure proper cleansing preparation.
Michigan Medicine's Dietitian explained ways to help reduce the risk of colon cancer with healthy eating habits and exercise. It was recommended to:
 |
For the best results, your stool should become light and transparent,
like the example on the farthest right
|
- Maintain a healthy body mass index
- Exercise for at least 30 minute a day
- Avoid sugar -energy dense foods and drinks including alcohol
- Eat a variety of vegetables, fruits, whole grains, and legumes
- Limit red and processed meats
Grilling or smoked meats have also been shown to increase risk of cancer as charred or burned meat contains carcinogens. Also, the use of a multivitamin, calcium, and vitamin d supplement have been shown to help reduce cancer risk although should be discussed with your doctor.
As genetic counseling plays an important role in identifying hereditary conditions, it is also important for communicating with one's family members for their own genetic testing. We heard from a genetic counselor and a patient panel about their experiences talking to their family members about genetic testing and the assistance received from genetic counselors with family members.
Travis, with Hereditary Colon Cancer Foundation, shared his experience with FAP and ways to advocate for awareness and education of the hereditary colon cancer syndromes. Dr. Elena Stoffel closed the conference with learning about medical advances to prevent the need for chemotherapy such as immunotherapy and gene therapy.
The University of Michigan, Michigan Medicine Department made registration available for a research study of microbiome identified through one's stool and a genetic registry. My mother and I decided to register for both projects.
The
Family Microbiome Project looks at the bacteria among family households - families with and without Lynch or FAP. Although this project is currently enlisting family households, they are interested in individuals for a future research project.
The
University of Michigan Cancer Genetics Registry has enrolled approximately 6,000 individuals from 4,700 families. To enroll an individual simply needs to have a hereditary cancer syndrome or personal/family history that is possible for one. Enrollment includes consent, medical and family history questionnaire and potential for a blood or saliva donation for research purposes. One doesn't have to reside in Michigan to enroll. Those registered are also notified of events such as the Hereditary Colorectal Family Day. If you're interested in enrolling or learning more, contact Erika Koeppe by
email or calling 734-998-1274.
If you're in the Michigan area and interested in a support group for Lynch or FAP there are two support groups to choose from:
- Gilda's Club of Greater Grand Rapids - Alice 616-885-6426
- FAP and Lynch Syndrome Peer Discussion Group - Kevin 734-476-7425
My mother and I had a great time attending the conference and would encourage you to attend any future conferences for networking and educational purposes.
It was incredible being in a room with so many others with the same condition at once!