Monday, December 10, 2018
What We Need From You
Chronic illness is a challenge, period. It's a challenge for those who live with the illness on a daily basis, for caregivers of the ill person, and for those who are involved with the person outside of the home. Chronic illness often leaves those in its wake feeling frustrated and helpless. The ill person struggles to live daily life with the symptoms of chronic illness and friends and family are limited on what they can do to help the ill person. To make matters worse, those of us with chronic illness are often hesitant to ask for help from others due to feeling burdensome and are frequently at a loss ourselves as to what may be helpful. To help all of us, here's a list of things we need from you due to chronic illness.
We need you to be available.
Chronic illness can be extremely isolating at times, particularly if it is a rare disease. Depending on the diagnosis, it can be difficult to identify and communicate with others with the same illness. Social media has helped close the distance among individuals with the same illness but in person visits remain different from online communications. We are further isolated due to difficulty to physically leave our homes except for our medical appointments. Even when we want to visit with others we may not physically feel up to visiting regardless of the communication form. We frequently experience hospitalizations and may only experience encounters with medical providers. Your presence in person, on the phone, or online is a tremendous support to us when we are able to do so.
We need you to listen and encourage.
Due to the elevated risk of isolation among those with chronic illness, we are at higher risk for depression. We easily become frustrated, discouraged, and depressed regarding our health issues and daily struggles. Your willingness to listen to our concerns and to encourage us along the way has an immense impact on our mental health.
We need you to be understanding and forgiving.
Changes in our health and abilities often causes us to feel angry and frustrated as we are adjusting to chronic illness. Furthermore, when we don't feel well we may be ill tempered. We don't mean to direct our frustrations and anger toward others. A gentle reminder when we are acting unfair will help us to realize any damaging behavior and allow us the chance to correct any harmful behavior. Your understanding and forgiveness is paramount in this process.
We need you to help us feel accepted and loved.
Chronic illness typically means changes to our bodies and abilities that may not be visible to others but we remain acutely aware of such changes. We may have difficulty accepting such changes and become insecure and self-conscious of our bodies, symptoms we are experiencing, abilities, and our self-worth. We all want to be accepted by others and this desire may be heightened by chronic illness. Your acceptance helps us to accept ourselves when we are struggling with self-love and acceptance.
We may need your physical assistance.
Chronic illness is high maintenance requiring ongoing medical management that includes frequent medical appointments, tests, procedures, medications and more. These tasks are demanding physically and mentally. As abilities are challenged by chronic illness, we may require your physical assistance in the form of transportation to appointments, assistance obtaining and taking medications, household chores such as cooking, shopping, and cleaning. Changes in our abilities often leaves us feeling as a burden on others resulting in our hesitancy to ask for physical assistance even when it is greatly needed.
We may need you to help us find assistance.
Chronic illness can easily create financial difficulty due to inability to work temporarily or permanently. Our finances may easily be overcome with medical expenses. Locating appropriate resources is not an easy task when one is sick. Therefore, your assistance in locating and applying for resources may be of great service to us during a time that we are having difficulty physically or mentally functioning.
We need you to help advocate.
As a patient, we benefit from advocating for ourselves but your advocacy on our behalf would also be advantageous. We may not always have the physical fortitude to speak up or we may forget questions to ask. You can help us by attending appointments with us and listening to the information presented by medical providers. Additionally, advocacy efforts on a larger scale directed toward public awareness and legislation are stronger with participation by patients and loved ones.
We need you to help us enhance our physical comfort.
Chronic illness often is exacerbated by physical symptoms that are distressing and even painful. We've learned little tricks to help ease our discomfort such as using heating pads, rubbing a painful body spot, or even taking a nap. When you are near, you can help by handing us objects such as a heating pad or our medication so that we may limit our movements, particularly when movement is painful. Sometimes a gentle rub on the afflicted body part or even something as simple as playing with our hair can be soothing. We often fight fatigue that negatively affects our sleep schedules. In such cases, helping us limit our nap time will help us maintain an appropriate sleep schedule while boosting our energy.
We need you to take care of yourself.
Lastly, we realize that providing care and comfort to a chronically ill person can be difficult on others and want your well-being to be taken care of as well. Caregiver burnout can be detrimental to all involved and the last thing we want is our illness to be harmful to you. We understand that one cannot provide around the clock care for us and maintain one's own well-being. Self-care is important for everyone, not just those with chronic illness.
We may not say it enough but all your efforts to support and assist us in the walk of chronic illness is greatly appreciated and we are far better off with you in our lives than without you. We thank you for all your efforts.
Labels:
Caregivers,
Family,
Health,
Support
 This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
Saturday, October 20, 2018
When Chronic Illness is a Deal Breaker
It was only about an hour of my time, he had already asked me out on a date. But that all changed when I told him about my health. I've never had someone point blank tell me my chronic illness was a deal breaker for them. My boyfriends and friends have always been supportive and understanding of my health issues. I've been fortunate to surround myself with empathetic individuals.
I do not know what his reasons were nor did I care to know. I knew what was important, it was a deal breaker and although taken aback a bit, I was glad to know sooner rather than later and I hadn't wasted that much time on our conversation. My first thought though was "I'm glad this happened now and not when I was a teenager or young adult". I had my ostomy when I was 9 until I was about 15. Growing up with an ostomy was very difficult for me emotionally and mentally. My self esteem suffered greatly under the pressure of growing up with an ostomy and later it would be an issue after my ostomy reversal and dealing with Short Bowel Syndrome. I was not as confident in my body or my health issues nor was I as honest and upfront about my health as I am now. How devastating it would have been for my fragile ego as a teenager or young adult to be told that my health made me not good enough for a relationship. Now I realize this is not a reflection on me but on the person making such a statement and so I am merely grateful to have that person out of my life.
It also worried me about this person in particular as he cares for children as a nurse practitioner in a children's emergency room. If he could be so non-understanding with an adult, how is he treating his young patients for their health issues? And what about his future partner as her health declines over time? My heart ached for these people affected by his poor attitude toward illness. I escaped with very little time invested but my well-being is not in his hands.
Working in healthcare myself, I look forward to romantic interests and friendships with other healthcare professionals as we are accustomed to dealing with illness and all the usual worries individuals have about illness and symptoms can be put aside with healthcare professionals. Evidently this is not the case for all healthcare professionals but I still believe it is with the majority of us. Most of us are desensitized to symptoms of illness and disease and so we can let our guards down with one another. I suppose with any other field or persons, there are good ones and bad ones.
If you are confronted with a person who decides your worth is not deserving due to your illness, I encourage you to not take it personal and try not to let it affect your mental well-being as this is a pure reflection on that person and not on yourself. You are greater than this judging person. You are worth a lot and deserving of all the love and kindness in the world just like anyone else. Your illness does not detract from you as a person. If anything, it adds to you as you are a survivor with wisdom and strength others are not privy to with their good health. Hold strong in yourself and shrug off the haters.
Labels:
Health,
Relationships,
Symptoms
 This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
Saturday, September 29, 2018
When Caregiving is a Vacation
I didn't realize what was happening until it was too late. I didn't recognize that I was staying in a toxic relationship until I just couldn't take it anymore. The end was perfect timing for a family cruise vacation to Hawaii. It was going to be a perfect mental health cleanse. Only it didn't happen. We experienced passport issues at the airport which prevented us from reaching the cruise ship and embarking on a lifelong dream with my parents. I was completely devastated upon this discovery. We had been planning this vacation for over a year. My heart broke as we left the airport to return home.
I turned to my friends for comfort and as it turned out, one was due to have knee surgery the following week. I offered to be his caregiver for a week. It wasn't the vacation I expected but it turned out to be something we both needed.
I drove to Colorado and arrived the night before his surgery. We enjoyed dinner out before returning to his home to prepare our overnight bags for what originally was to be an inpatient surgery. I've never really been on the caregiving side so this was to be a new experience for me. I've never waited in a hospital waiting room for someone else undergoing surgery or procedures - it's always been me as the hospital patient. We woke up early on surgery day and made our way to the hospital. I stayed with him until they finished prepping him for surgery and anxiously waited in the waiting room for the surgery to be completed. Finally, the surgeon came out to update me on a successful surgery. With relief, I waited for him to be stable enough in recovery for me to join him. Unfortunately, he had a bit more difficulty coming out of anesthesia and some nausea issues from the pain medicine. These complications delayed our reunion in recovery by a couple hours. While waiting, I updated his family members on his condition until we were finally able to return to his home.
 |
| Aspens starting to change color |
We were finally released after the inpatient admission changed to outpatient. We returned home and I was officially a caregiver now. I made sure he had food and drink, his medications at the appropriate times, and did all the little things he needed done while recovering. Just like with anyone in pain and recovering from major surgery, there were times he didn't feel well and it showed emotionally and verbally. I shrugged it off - knowing that I had been the same way after my surgeries. For the next few days we remained cooped up in the house except for when I needed to run errands for him. He asked me to stay an extra day and when he was feeling more like himself, we enjoyed an afternoon road trip through the beautiful Colorado mountains, before my departure the following day.
 |
I didn't mind being cooped up in the house. I was just grateful for not only being able to spend time with my friend but also the break away from my life back home. Nor did I mind providing care to my friend, running errands, and getting up multiple times during the night to help him as needed. My time as a caregiver was only a week and I appreciate the difficulties and strain that accompanies caregiving - particularly long term caregiving. I enjoyed my time as a caregiver. It became a blessing in disguise as we both needed my presence there. He needed a caregiver and I needed the time away from my life.
I left my friend to return home knowing that the worst part of his recovery had passed and my mental health had improved. We were both grateful for the time and care we provided to each other - me as a physical caregiver and him as an emotional caregiver.
Labels:
Caregivers,
Travel
 This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
Sunday, August 26, 2018
A Love Hate Relationship with Medicine
I have a very tumultuous relationship with the medication Lomotil, generic is Lonox. This relationship changes periodically throughout the years. I take Lomotil to slow my bowel movements due to my Short Bowel Syndrome. The amount of Lomotil I require has also changed throughout the years in relation to how my body is affected by the medication.
During the 6 years that I had an ileostomy, I never took Lomotil. However, when I was able to have my ostomy reversed in high school, I required Lomotil to slow my bowels and help with my control. I started off requiring 4 pills a day and I would take these all at once in the morning and they would last throughout the day. I don't remember noticing any negative side effects such as increased pain or cramping. As that first year progressed so did my adhesions causing a stricture. I endured daily vomiting and excessive diarrhea that required surgery to remove the adhesions causing the stricture. For a period, I not only required Lomotil at maximum dose but also Sandostatin shots. But none of it worked to slow my bowels. I had a negative side effect to the Sandostatin after a while - it caused my elbow to lock. And I was forced to rely on the Lomotil by itself. Gradually throughout a year as I prepared for starting college, my body adapted once again and the Lomotil became sufficient in its job. Due to manufacturing changes, I had to change from the generic form to the brand name for continued efficiency. I managed throughout college taking the maximum dosage and remaining active, completing all the activities I wanted with minimal difficulty.
With my first full time job came new insurance that didn't cover the brand name and I was forced to change to the generic form of Lomotil. Manufacturing must have changed or my body changed once again as the generic form was now sufficient. And then I was suddenly able to decrease the amount I took until I was able to stop it all together for the most part. When I was having a particularly busy day I would take some, varying on the amount based on my activity for the day. As the year progressed with this job so did my stress level. The intense stress of my job wreaked havoc on my body and Lomotil was no longer sufficient even at maximum dosing - my Short Bowel Syndrome was out of control and I had to quit my job. I took time to heal and lessons from this job experience to better cope with future job stress without the bodily toll. Over time, I was able to stop the Lomotil once again and only take it as needed for particularly busy days.
Now, almost 10 years later and I have new problems - increased adhesions. My adhesions cause chronic pain and nausea and I hate taking Lomotil as it increases my pain while slowing my bowels. And if I take too much Lomotil for too long of a period, I risk intestinal blockage. So now I only take Lomotil when I'm having a Short Bowel flare or when I'm going to be particularly busy, such as for an outing or on vacation. I judge the day's activities and bathroom access for determining my dosage for the day. When I'm on vacation, such as on a cruise, I will take maximum dosage as I am very busy during these vacation. If I'm going on an outing, I may just take one or two pills.
The side effects of my Lomotil with my adhesions often causes me to dread outings and activity although I enjoy the activity itself. It's a hard balance to obtain between the bloating and pain that's increased by taking Lomotil with making sure to find a bathroom with any activity. My body seems to undergo periodic changes and so I await to see how it will fare over the next few years and what changes are on the horizon.
Labels:
Activity,
Medication,
Short Bowel,
Symptoms,
Travel
 This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
Saturday, July 28, 2018
Protecting the Heart Against Anemia
I've struggled with iron deficiency anemia since I had my colon removed in June of 1995. I was soon started on iron tablets, one with every meal. This managed my iron with a low normal hemoglobin for years but I was never able to reach the desired 14-15 hemoglobin my pediatrician so desired for me. Two decades later when I unexpectedly hospitalized in May of 2015, I left the hospital with increased chronic pain and nausea. My new doctor directed me to stop my iron tablets, stating they were contributing to my pain and I didn't need them anyway. Well, I did need them and I was referred to a hematologist for iron infusion therapy. My hematologist also advised me to switch from iron ferrous to iron gluconate, as the gluconate is easier on the stomach. Although I still have chronic stomach pain, it is reduced with the iron tablet switch. Why would I take iron tablets still if I'm getting iron infusion therapy? Why to prolong the time in between iron infusion treatments. It has helped, I required iron infusions every 3-4 months.
So why do we need to worry so much about iron? Not only does it have bothersome short term symptoms but there are also long term dangers if left untreated. Long term effects I didn't even know about until I started researching.
When we're anemic, our bodies are unable to produce the required amount of red blood cells we need to carry oxygen throughout our bodies to all our organs and body parts. These red blood cells also carry carbon dioxide out of your body to be exhaled. To create red blood cells, the body requires nutrients such as Folate and B-12. So it's important to have these levels checked as well.
Iron deficiency anemia is common for those missing the colon and/or part of the small intestine. Symptoms include:
- Fatigue
- Weakness
- Pale skin
- Irregular heartbeats
- Shortness of breath
- Dizziness or lightheadedness
- Chest pain
- Cold extremities
- Headache
What I didn't realize though about prolonged anemia, is that it can cause heart problems. Remember, that short term effect of an irregular heartbeat? Prolonged it can cause arrhythmia (rapid, irregular heartbeat) which can lead to an enlarged heart or heart failure as the heart is weakened by overworking to pump more blood than normal to compensate for a lack of oxygen in the blood. This can lead to other bothersome symptoms, additional serious medical conditions, and death.
Signs and symptoms of heart failure include
- Shortness of breath
- Fatigue
- Weakness
- Swelling
- Arrhythmia
- Persistent cough or wheezing with white or pink blood phlegm or mucus
- Increased urination
- Ascites
- Rapid weight gain from fluid retention
- Lack of appetite and nausea
- Difficulty concentrating
- Kidney damage or failure
- Heart valve problems
- Liver damage
- Diet changes for foods rich in Iron, Folate, Vitamins B-12 and C
- Supplements for Iron, Folate, Vitamins B-12 and C
- Iron Infusion Therapies
- Any other recommendations
If you have iron deficiency anemia, I promise getting treatment to properly manage your iron levels will make you feel tremendously better. As much as I hate needles, I love my iron infusions.
Labels:
Food,
Health,
Medication,
Procedures,
Symptoms
 This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
Saturday, June 9, 2018
A Look at Caregiving
This is a Guest Post by My Father
My daughter asked me to write about my experiences as a caregiver to herself and her mother. It made me contemplate for a while as I really don't consider myself a caregiver. In my heart, I am just a husband and father doing what those roles routinely require and the fact that my wife and daughter are chronically ill is just another dimension to my husband and father roles.
Cambridge Dictionary defines a caregiver as "someone who provides for the needs of people who are ill or can't provide for their own needs". So, okay, I guess I am a caregiver even though I consider my role more of that as a husband and parent. I don't consider providing health related service to my family any different than changing diapers for my daughter when she was a baby, it's just one of those things you do. My wife is fond of saying "You do what you need to do".
I also provide service for my wife and daughter beyond their illnesses wherever they need support. For example, my wife required a new car battery. I completed the task at hand as she was in need of assistance and she has a weight lifting restriction. I tend to categorize my service as things that need to be provided because I am the best source not because of their chronic illnesses. I complete certain tasks that are beyond their individual skills or abilities, it is more than I expect them to do. They are health related although I didn't consider the health portion in my willingness to complete such tasks.
A lot of routine husband and parent duties are health related but a lot are just duties that aren't necessarily required because of chronic illness and others cross categories. I complete required maintenance of our homes as well as medically required tasks such as my wife's daily eye drops, transportation to medical procedures, or picking up prescriptions. My daughter was on TPN for a while during her high school years and my wife and I were both taught how to provide care for her central line and feedings. It became a priority item in the daily routine and we tried to make it a fun activity and family bonding time rather than a time of an unwelcomed dreaded chore.
When we first realized that my wife would be facing a life time of health issues related to her Familial Polyposis and Type II Diabetes diagnoses there was concern on my part about the amount of daily time this would require of myself. In retrospect, it hasn't been much different as the extra work involved became part of being an actively involved family member. There are always things that need to be accomplished on a daily basis and the health related items fit into normal daily activities quite well. It's all part of being an active family member.
Chronic illness is a day by day process that can bring a lot of frustration, anger, depression, and angst for the patient and the family. Being the regularly healthy one in our family trio means that I need to just be a stable, dependable source for the needs that arise on any given day. It may be a comforting hug, a kind and supportive word, a ride to the ER, or taking out the trash and preparing a meal. Because my health is stable, I can provide such services as a caregiver with little burden or difficulty.
An attitude of welcoming the opportunity to serve rather than resentment of each chore is an essential ingredient in creating a healthy, mutually respectful and loving relationship between caregiver and recipient. Using the time to strengthen bonds, deepen the relationship and draw closer together instead of letting it draw apart and create barriers. Chronic illness is generally no one's fault, it just is; it's something to learn to live with as best as you can regardless of your role. We live day to day, appreciating the good days that are available to us. Being supportive, encouraging, willing and happy to serve, being a support that can be depended upon regardless of the time or day. Instead of considering the extra health related duties as unwanted chores, consider them an opportunity to serve a loved one and perform that service with humility allowing it to be a time of comradeship and an enriching quality time.
Being helpless to improve the situation, feeling guilty as the healthy individual and they aren't, being stretched and stressed can be a daily issue for a caregiver. Utilizing those healthier times to enjoy life together helps to relax and unwind, to reflect and re-group for one's physical and mental well-being is important. Being thankful daily for where you are at this time and place is a good way to quantify the caregiving role and the rewards that are received in performing service to others. Because at the end of the day, as my daughter reminds me with her request for this article: I am a caregiver and I'm honored to have such a role.
Labels:
Caregivers,
Family,
Guest Post
 This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
Saturday, May 26, 2018
False Hope
With the changes to my health over the last two years, I can't help but believe that this is the healthiest I will be. Actually, in truth, I believe my healthiest days are behind me and this is my new level of healthy - a step down from where I was and therefore everything else that is to follow will only be worse.
All in all to try to fix the problem of my declining health over the last two years, I've endured 3 upper scopes, 1 lower scope, CT scan, labs including stool specimen testing. And although things have been ruled out as culprits and some culprits have been found, the underlying issues remain - I have chronic nausea and pain. And perhaps this is all primarily from the adhesions as my doctor diagnosed last year. Even if this is the case, the fact then remains that it will worsen as the adhesions continue to worsen and surgery for adhesion removal is inevitable - and so are risks that come with such surgery.
I lived with an ileostomy for six years before I was finally able to have my ostomy reversed with a straight pull through. Reversal wasn't a guarantee for me and whenever there is a surgery involving my remaining intestine, there will be risk of another ileostomy - only truly permanent this time.
 This is my fear for the future. Although better equipped to adjust and accept an ostomy now versus when I was a teenager, I still do not prefer an ostomy. With all the problems that my straight pull through has with the development of short bowel syndrome, I still do not regret my decision for reversal and I want to maintain my reversal.
This is my fear for the future. Although better equipped to adjust and accept an ostomy now versus when I was a teenager, I still do not prefer an ostomy. With all the problems that my straight pull through has with the development of short bowel syndrome, I still do not regret my decision for reversal and I want to maintain my reversal.And to further complicate my health, I was recently diagnosed with Acquired Polycystic Kidney Disease. I don't have a family history of Polycystic Kidney Disease and haven't undergone genetic testing for the gene so it is assumed that it is a sponatenous manifestation within me. My nephrologist advised I have an estimated 20 years before I start to experience kidney issues, which at that time it will be likely that my kidneys will start to fail from an abundance of renal cysts and will require kidney transplant or dialysis if I want to continue living. My nephrologist advised that due to my Familial Polyposis, I am greater risk of cysts and cancer occurring. And so I will be monitored once a year with a CT Scan to monitor for cysts and tumors on my kidneys. As long as I can stave off my GI issues from worsening, I have an estimated 20 years of health remaining before I will begin to experience another change in health.
I struggle with this reality and with the present. I'm told to not give up hope for improvement of my symptoms. But at some point, false hope can be dangerous. I want my health to improve and perhaps it will but the odds are, this is it for now. I'm remaining open to trying a few more things but I'm trying to balance myself between positive hope and false hope. I've learned that when we cling to false hope, we are hit hard with a different reality. A reality that we could have been better prepared for if we had accepted the chance that exists for what we fear.
 This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
Saturday, May 12, 2018
When I'm Asked How I'm Doing
When you have a chronic illness, sometimes it's hard to know how to answer when asked how you're doing. The odds are, we're not doing very well. We have daily symptoms we're contending with and most of the time we don't feel well but we don't want to admit that to others. We question the sincerity of the question and what is considered to be too much information when we answer. So we lie usually instead of answering the truth - the truth being that we aren't doing well.
I always question does someone really want the truth or just the brief, expected answer so that conversation can move along. I rarely answer honestly. I entered the habit of answering "okay" or "good" even though it was a lie. I was tolerating the moment even though internally, I felt like death warmed over.
I became tired of answering with a lie and a superficial glancing over my daily health. I wanted a more sincere answer but I also didn't want to dwell on the answer, particularly if my well being is only being sought after on a superficial level, out of societal nicities. I hate the looks of pity when I answer with a truthful "I'm doing horrible" type of answer.
I tried out different answers that felt genuine for me but none felt right. To say I'm functioning is true but it invites additional questioning and feelings of pity I thought. I'm alive didn't work well either for me. I finally settled on "I'm hanging in".
I'm hanging in provides a truthful answer without the invite for pity from others. It allows for further conversation but doesn't require additional questioning. It's clear and to the point - I'm managing but I could be doing better but I'm not worse either.
How do you answer others when asked how you're doing? What have you found works best for you? Share with me.
 This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
Thursday, April 26, 2018
What I Learned From Divorce
When I divorced, I never could have been prepared for what to expect. No one tells you what you should expect, there is no handbook. Your world is turned upside down and you feel like your life is out of control. You simply live in trial and error and commiserate with other divorcees who can relate to your experiences. There is so much you learn during this period that can last for years even. The navigating, the learning may never cease. I'm only two years post divorce and although my married days feel like a lifetime ago, they remain with me although diminished in intensity.
From the initial moment I made the final and clear decision to end my marriage I began to experience an exhilarating time; I was filled with emotions of relief that were freeing to my mind and soul. I no longer had to hold on to the stress and worry that had accompanied me for the months previously while I battled depression and the stress of trying to hold on to everything while maintaining my sanity. With all this freedom, my energy levels soared as I was no longer burdened by immense stress. I started exercising, I could hardly sleep due to my abundance of energy and my excitement for the possibilities of the future. I felt limitless and carefree, unburdened by my final decision.
I began to re-enter the dating world shortly after, as is a common occurrence. Looking back, I realize now that a divorced individual is a mess for at least a year following the divorce and for that person's own sanity and sake, really shouldn't enter into relationships during this time. Refraining from re-entering the dating world for a year would be a very difficult commitment for most individuals. As humans, we long for companionship and intimacy with others. We tend to enjoy the thrill of finding potential new partners and participating in the dating realm. We feel desired by others giving us attention after an ordeal such as a divorce. The options for potential partners is an exciting new world that is reopened to us. It's a thrill that is hard to deny. The first year particularly is for a time of healing and rediscovering one's self. I had an intense amount of energy and drive for my limitless future but my mind was so scattered and pulled apart by all the options that now laid available to me. My mind raced between options and even though I set goals and plans for myself, I didn't stay with a plan for long before racing to another idea and option. It must have been exhausting for anyone listening to my rambling ideas and trying to keep up with my racing mind. Just as I wasn't ready to commit to another relationship, I wasn't ready to commit to even a singular life plan.
I was not ready for an emotionally invested relationship. I began to become terrified of relationships and kept a cold, emotional distance between myself and others. I've never had a great record of dating and I figured this time around wouldn't be any different; only this time I wouldn't marry again. I would forever be entering and exiting dating relationships. I vowed to myself that I would never allow myself to become lost to another, I would maintain my physical, financial, and emotional independence from another. Relationships became an "easy come, easy go" mentality for me as I kept distance between myself and a partner. I began to view relationships as impermanent. I survived what I thought I wouldn't - losing the person I considered my soulmate and life partner. If I could survive that and be happy again, then the same is true for any future relationship; I will survive any relationship ending. I wouldn't allow myself to become overly emotionally invested and as a result, a failed relationship was merely an inconvenience that could soon be replaced by another potential suitor. I spent a year dating men younger than myself and I learned to appreciate men who were closer to my own age. Not only was I not emotionally available but I also didn't want to deal with immaturity or drama. I had experienced enough drama with my own divorce, I didn't need or want additional drama brought into my life by another individual. I wanted simplicity and partners who themselves were an emotionally strong individual. I was tired of being the emotionally strong person all the time. I wanted someone who could stand their own. Although I have allowed myself to find a deep love again with the intent for building a lifetime together, I maintain a conscious eye on my independence. I've learned that with the right person, I don't have to keep a cold, emotional distance between ourselves as a means to protect myself. I can let another into my heart and remain independent and maintain a healthy self. Becoming cold and distant does not make a healthy relationship and now that I've re-opened myself to a deep and loving relationship, I am much happier than I was in previous relationships. In spite of finding a deep love, for good or bad, without any effort I maintain the view of relationships being impermanent.
While navigating the divorced world, I realized that all my new moments are tainted by past memories and experiences during my marriage. This has lessened with time, but there are stinging moments that cross my heart as I remember a time with my now former spouse or when I am embarking upon a new adventure that would have been with my former spouse if divorce had not occurred. It was quite painful as such events would trigger a flood of memories and grief over what was and what was supposed to be. I had a difficult time coping with vacationing and buying a home on my own rather than with my former spouse. I felt as though everywhere I turned, there was a tainted moment that should have been experienced with my former spouse but now was my sole experience. The sting has diminished in intensity and length, but it remains even though fleeting as it is.
My life changed drastically upon my decision to divorce. I gave up a lot but gained a lot in the end. Divorce was not an easy decision; working my way to that final decision was soul wrenching and I spiraled in a well of anger and depression. It was not an easy transition to make, the transformation of myself couldn't be rushed. But as my heart and mind began to heal though from the aftermath, I've come to love my life and everyday I am grateful for this new, even surreal life.
The upheaval of divorce varies from person to person and situation to situation. This may be
exacerbated any time divorce is contested or involves minor children or property. The entanglement of finances alone can cause extreme stress and friction.
Even when you do your best to maintain independent finances and property from your spouse, I learned that there is always entanglement. If your spouse has financial difficulties, it can be linked to you even when you didn't share finances or property. With this ongoing entanglement due to a previous legal connection to an individual, I realized I wished I had changed my phone number after the finalization of divorce. Years later and I still receive random phone calls connected to my former spouse.
Fortunately my divorce was civil; we even said we would always be there for one another if the other needed. Perhaps this was naivety and wishful thinking in the freshness of our separation. We still have one another's phone numbers and whenever I have questions about anything, he's always willing to provide answers. But would I be able to truly count on him if I needed something? I'm not so sure of that now with the passing of time. Perhaps but perhaps not. With all our civility and promises to one another, I was shocked when I suddenly discovered he had removed and blocked me from his social media platforms. I should have expected it. We weren't what anyone would consider friends anymore. But it was still a shocking realization for me. With one less person in my support system, I had to accept that I may need to lean on my existing support system more heavily due to my health but I also needed to be more independent myself. Our mutual friends now became his and mine; I no longer had his family and friends to call on.
Divorcing was a heart wrenching decision but ultimately it was the best decision for me. It would have been nice for things to have turned out differently, but they didn't. For myself, I must let go of any regrets and instead find my peace and enjoyment in everyday life wherever and whenever I can as I navigate the divorced world.
Other divorcees shared with me what they wish they had known to expect or what they had learned from divorce. See what others had to say:
- When dealing with property there is the risk of both individual's credit being ruined.
- Splitting up pets can be emotionally wrenching. - Wendy
- You may end up taking care of the children all by yourself - Joe
- You learn who your true friends are and there may not be as many as you thought there were - Tricia
- Sometime it's worth asking "is it more important to be happy or to be right?" when considering remaining in a marriage - Amanda
- Men and women react differently. Where one may act devastated the other may act in the complete opposite. For example "I was devestated and upset, he behaved in a very matter of fact way, was switched off from me completely and had metaphorically closed the door on me and our relationship. It was as if I suddenly had no part in his life or in his relationshp with the children". - Lynley, Top Lady Talks
- You lose friends, other women may look at you as a treat to them even though you did nothing wrong in the relationship, and it took bravery to walk away - Bree
- "I lost a lot of things but my mantra was 'I have my freedom'!" - Aileen
- "It's the kids that matter the most, to make sure they are treated right and always told that they're loved." - Amanda
What are some lessons you wish you had known prior to divorce?
Labels:
Divorce,
Mental Health,
Relationships
 This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
Thursday, March 29, 2018
Living for Work
My pediatric GI doctor talked to me and my parents about my chances for Social Security Disability (SSD) Benefits to ease the financial burden associated with my chronic illness since I was a child. I grew up hearing about how I would be able to obtain SSD benefits if I applied. My parents opted to never apply for SSD benefits for myself as they didn't want me to see myself as different from other children and teenagers and were fortunately financially able to withstand the financial burden my health placed upon them.
For me, SSD benefits was never an option truly placed upon the table but I also knew that my doctor and my parents hoped I would be able to physically complete my schooling and obtain full time employment and become a financially independent person - but that this was not a given but rather a hope as none of us were sure how my health would withstand the such physical stress.
So I put forth my full effort into the tasks of life. My parents home schooled me for a year in grade school due to my health not allowing me to meet the attendance requirements of public school during the first year of my surgeries. And in high school I risked inability to graduate on time during another physically trying year with medical tests, procedures, surgeries, and multiple hospitalizations. I was only able graduate high school due to the kindness of one of my high school teachers agreeing to tutor me during my home study absence period.
In college, I endured regular hospitalizations due to difficulty maintaining my electrolytes. My college professors worked with me to allow me to complete my assignments and exams around my hospitalizations as needed. My health stabilized the year I graduated college affording me attendance to graduate school and my practicums with minimal difficulty.
However, when I started my first full time job the stress would become too much for my body. I was traveling around the state on a daily basis, even to the borders of my state on a bimonthly basis. My employer was not overly accepting of my health. After consulting with my parents about my health and financial situation, I was forced to resign for the sake of my health.
I was not defeated though. I allowed myself a month of rest before re-entering the work place with a different employer. I had learned new ways to cope with the stress of full time employment and how to deal with an employer. I succeeded at maintaining my health even when this employer entered the realm of a hostile work environment. I found a new position with yet another employer who works with me on my health issues and have been able to maintain full time employment ever since without difficulty for 7 years now.
With abrupt health changes over the last two years, especially during this year, I began to worry about my ability to maintain full time employment. Without my employment I would become dependent upon attempting to obtain SSD benefit approval and assistance from my parents in the meantime. SSD benefit approval is not necessarily an easy task to achieve and can take years. Even after approval, you are often required to wait another two years for Medicare health insurance to become available.
My greatest fears in life include not being able to financially support myself and to become nursing home dependent or homeless and to be able to care for my parents as needed. When I was married, I was less fearful of these risks as my home was a two person income home. However, I had to weigh the financial risks I could potentially be under when I divorced. When I divorced, I was accepting that I am solely responsible for my financial well-being regardless of my health. I would be at greater risk of my greatest fears becoming a reality if unable to maintain employment. When I divorced, I learned a new level of independence that I vowed to fiercley protect and cherish for all my days on Earth even if that I meant I had to work until my death. No longer would I allow myself fairy tale dreams of being a stay at home wife - I would forever be a working woman for as long as I required and am able.
And with this new attitude and determination, I admit that I live to work. It's not out of enjoyment or because I'm a workaholic but rather out of necessity for my surival and mental sanity. My health has always been unpredictable causing my future to be unpredictable. I will ferociously hold onto the few things I can control in my life with an intense tenacity. It is due to this outlook, that I dismiss others when they say it's no life to live to work. For others this may be true, but it doesn't hold true for me. Rather, I increase my ability to survive physically and mentally when I focus on maintaining my employment ability for as long as I am able - even if that means I work past retirement age. The more I work, the more financially stable I become, the more I am able to prepare for the uncertain turns my health will take that is chronic illness.
Labels:
Employment,
Health,
Survival
 This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
Thursday, March 8, 2018
Life with Chronic Nausea
Nausea is easy to understand, right? It's simply of feeling of sickness with the inclination to vomit. Seems pretty straight forward. Not so much for me though, at least not my chronic nausea.
For me, chronic nausea is something different than just the inclination to vomit. It's different from nausea that can accompany a stomach virus, food poisoning, or over indulging on alcohol. I don't typically even vomit from my chronic nausea. My mouth doesn't start to salivate in preparation for the impending upchuck, I don't start heaving, I don't have to stop talking or risk vomitting. None of the usual signs I experience when I'm inclined to vomit. No, typically if I were to vomit from my chronic nausea, it's because I forced myself not because my body forced me. Although, frequently I wish I would vomit when I'm nauseated as I believe it would help provide relief. This is a predicament I find myself struggling with regularly and unfortunately, not new to me.
Instead of the typical response to nausea, my whole body reacts to my chronic nausea. My nausea has various triggers and although I can usually predict when the nausea will hit based on my behaviors, it is not always known to expect it crashing in upon me. Ingesting food or liquid often triggers the nausea as it fills my stomach and causes discomfort or if I become overheated I will become nauseated. Other times physical or visual motions will send me overboard. The slightly shaking is too much for my stomach and at times even the movement of a computer mouse or the scrolling of a computer screen will act as a trigger. And even with these triggers, there are times that I will simply awake nauseated. But whatever the reason for it, it always feels the same.
Typical nausea that subsides upon the expultation of the irritating source, I would welcome that. But that is not my experience. I can usually feel the nausea crashing over my body like the waves of a tide. I feel like complete and utter rubbish when the nausea hits. My body has a generalized, overwhelming sickness to it; my stomach hurts and feels uneasy, I feel full and bloated. On particularly worse occasions my head will slightly hurt and if I close my eyes to rest, I feel as though the room is spinning about me. I feel as though if I could just vomit or empty my bowel, I would feel better. I have the urge to lie down in a ball and hold onto my stomach. At times it becomes too much and the tears fill my eyes as I'm overcome with frustration at my physical status.
I regularly utilize my anti-nausea remedies- Compazine and Phenergan tablets, peppermint candies, and Peppermint Oil. I even have Phenergan gel as well. But nothing makes the nausea dissipate immediately, it's a gradual overthrowing of the nausea. And in the meantime, I'm left wanting to make myself vomit in an effort to make it stop yet knowing that it's not healthy to make ourselves vomit.
The chronic nausea is there with me, almost every day without warning, it is never cured. It's simply managed and so I must continue functioning in spite of the discomfort. I can't stop living my life or completing my responsibilities over nausea. In spite of my efforts to fight through the nausea, there are times that it is simply too overwhelming and all I can manage is to rest. But it sure would be nice to return to my pre-chronic nausea days.
 This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
Thursday, February 15, 2018
Probiotics and the Immune System
I attended a seminar about Probiotics, Food, and the Immune System presented by the Institute for Natural Resources. This is just one of the many topics INR Seminars provides for healthcare professionals. The material is written by an expert and then presented by various educators. This particular seminar's syllabus was written by Dr. Nikita Katz, M.D., Ph.D. and was presented by Dr. Laura Pawlak, Ph.D., R.D. emerita.
This 6 hour seminar covered an intense amount of information about how the immune system works and is affected by foods and probiotics (healthy bacteria) with a specific focus on pro-inflammatory and anti-inflammatory influences. I will not be going into as much detail as the seminar provided.

Dr. Pawlak began by explaining that in the big picture there is a reciprocal interaction between food and environment on the immune system and on an individual's microbiota that then may affect the brain. The particular focus was placed upon the effects of pro or anti inflammatory properties that may protect or hinder the body as genes become expressed and diseases occur. Food and the probiotics that are found within our food or through medicinal supplements impact these protective or harmful factors and how our immune system functions.
Probiotics are commonly recommended for individuals with digestive disorders or diseases to help maintain a healthy gut flora that is easily disrupted by digestive disease. Probiotics are also recommended to be taken following the use of antibiotics in order to help replenish the good gut bacteria that is stripped away by antibiotics. To understand the importance of probiotics, it helps to have an awareness of the effects of microbiota on the body and interaction with the immune system.
Our immune system is made to protect us against threats that are not considered "self". Typically, immune responses are elicited from viruses, bacteria, and parasites that cause infectious diseases but can also be prompted by our own cells that look different than expected, such as cancerous cells. Immune responses are aggressive and must be controlled as the immune system has the capability to kill the identified organism, or person, itself.
The human microbiota is a combination of microorganisms that includes bacteria, fungi and archaea. Some microbiota found within humans are beneficial to the body whereas others may be harmful. There is a delicate balance required for human microbiota and its essential role for a healthy immune system and various neurobiological functions.
The Human Microbiome Project found that there are thousands of bacterial types found within an individual and different body sites have their own distinctive bacterial communities. The specific bacterial makeup for a given body site varies from person to person by type and abundance. Due to each part of the body having a different microbial arrangement, different probiotics will target different areas. Not every probiotic will be helpful to every part therefore this needs consideration when selecting food and medications specifically for their probiotic benefits.
It's estimated that 500 to 1,000 species of bacteria live in the human gut. Gut flora has the largest numbers of bacteria and the greatest number of bacteria species in comparison to other parts of the body. These gut bacteria are predominately Firmicutes and Bacteroidetes but others present also include Proteobacteria, Verrumicrobia, Actinobacteria, Fusobacteria, and Cyanobacteria. The gut flora is established within one to two years after birth which is enough time to allow for the intestinal epithelium and mucosal barrier to support the gut flora and provide a barrier to pathogenic organisms. Probiotics help protect the mucosal surface barrier from inflammation. When this barrier weakens due to inflammation, resistance to malignancy is reduced and cancer and inflammatory disorders may occur. With weakening of the barriers, we risk microbiota leakage or absorption in between cells where we do not want absorption. The brain receives every nutrient introduced to the body and probiotics activate the vagus nerve that reaches from the abdomen to the brain. The blood brain barrier allows nutrients to reach the brain while limiting harmful substances reaching the brain. However, with weakening of the barriers due to inflammation, harmful substances may pass through the blood brain barrier.
Depending on our food choices, certain foods can help keep good microbiota alive and bad microbiota down and vica versa. Fiber and oils promote the good whereas sugar and fats promote the bad. You may notice this when constipation occurs as bad microbiota likes constipation. Once the diet falls apart, so does the immune system. Diet also influences the type of microbiota present. A healthy diet promotes healthy microbioata whereas unhealthy foods promote harmful microbiota. Nutrients are vital for efficiency of the immune system.
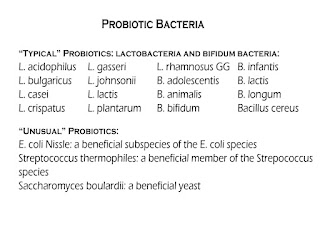 |
| Typical and Unusual Types of Probiotic Bacteria for Healthy Gut Flora |
Foods that naturally contain probiotic bacteria include:
Fermented cruciferous vegetables, fermented root vegetables and legumes, and sour milk products such as:
- Yogurt, recommended to be plain yogurt with no added sugar and labeled with live and active cultures. To sweeten, add fruit. Avoid adding sugar, artificial sweetners, or honey
- Kefir
- Icelandic skyr
- Swedish filmjolk
- Buttermilk
- Acidophilus milk
- Crème fraiche etc.
- Kombucha
- Kimchi
- Sauerkraut
- Green olives
- Tempeh
- Szechwan vegetable
- Indian pickle
- Mixed pickle
For the growth and activity of probiotics, prebiotics are necessary. Prebiotics are typically non-digestible fiber compounds in foods such as chicory root, Jerusalem artichoke, dandelion greens, garlic, leeks, asparagus, wheat bran, whole wheat flour, and bananas. There is not a broad consensus on an ideal daily serving of prebiotics but recommendations typically range from 4 to 8 grams for general digestive health and up to 15 grams for an individual with a digestive disorder.
There are diseases and syndromes linked to bacterial imbalance and immune dysfunction. These imbalances can occur in various parts of the body where the microbiota has deranged. In such instances, the normally dominating bacteria species become underrepresented and the normally outcompeted or contained species increase to fill the void. This dysbiosis, or microbial imbalance, is most commonly reported as a condition of the GI tract, particularly when there is an overgrowth in the small intestine of bacteria or fungi. This has been reported to be associated with illnesses such as periodontal disease, IBD, chronic fatigue syndrome, cancer, and colitis. It may be important to note that patients treated with PPIs to reduce stomach acid tend to have a higher frequency of small intestine bacterial overgrowth.
Microbes within a tumor can affect cancer growth and spread. Microbes and microbiota affect cancer formation by altering the balance of tumor cell life and death, immune system function regulation, and influencing the metabolism of foods and pharmaceuticals.
Mucosal surface barriers within the body require rapid repair, once these barriers are breached then microbes can elicit pro-inflammatory or immunosuppressive programs thereby allowing cancer and inflammatory disorders to occur. Probiotics can help protect the mucosal surface barriers against inflammation.
Inflammation is a biological response of body tissues to harmful stimuli and a protective response. Inflammation functions to eliminate the initial cause of cell injury, remove necrotic cells and tissues damaged from the original insult and start tissue repair. The typical signs of inflammation include heat, pain, redness, swelling, and loss of function. Inflammation may be acute or chronic. Prolonged inflammation can lead to a progressive shift in the type of cells present at the inflamed area. Inflammation can cause disease related genes to be expressed and is linked to most chronic diseases including arthritis, cancers, cardiovascular diseases, IBD, and diabetes.
Of the dietary components tested thus far on the Dietary Inflammatory Index (DII) for pro-inflammatory and anti-inflammatory properties, the top anti-inflammatory components include Turmeric, Omega 3 Fatty Acids, Fiber, Genisten (protein found in soybeans), Tea - the leaves are best, Alcohol - wine berries, and Magnesium. Turmeric should be taken with fresh ground black pepper in 10 parts turmeric to 1 part pepper for optimal absorption. the DII has a long way to go still as only a handful of dietary components have been tested for their pro and anti inflammatory properties.
When thinking of maintaining a healthy immune system, we must take in consideration not only the foods we ingest but also our exposure to environmental factors. With the advance of technology, we are now exposed to chemical compounds that were not naturally occurring on the planet previously and we are now exposed to chemicals normally hidden within the ground that are now exposed through mining and manufacturing. Heavy metals exposure causes significant alterations to the immune system by increasing the body's pro-inflammatory and decreasing anti-inflammatory responses. Air pollutants, pesticides, phthalates, PCBs, and perfluoralkyl substances exposure are also associated with medical conditions.
To help reduce one's susceptibility to immune dysfunction associated with such environmental influences, it's recommended to choose phthalate free personal care products, fresh foods rather than processed foods, and reduce exposure to pesticides, heavy metals, and air pollutants as much as possible.
To help lower inflammation and maintain a healthy microbiota balance, it is recommended to eat healthy, fresh foods, ingest probiotics, obtain adequate sleep , exercise regularly, and reduce stress. Exercise secretes proteins that are anti-inflammatory and remaining in the stressful fight or flight crisis response mode increases inflammation.
 This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
Friday, January 26, 2018
Lasik - Eye Surgery
Disclaimer: I will be sharing my experience with Lasik eye surgery and may be a trigger for those who are sensitive to medical descriptions.
I've dealt with nearsightedness for years. I required eyeglasses by the time I was in high school so that I could see the blackboard and once I started driving. It seemed as though with each annual eye exam, my nearsightedness worsened but I hate wearing eyeglasses or contacts on a regular basis. I feel as though I can't complete everyday activities outside of driving with my eyeglasses and wearing contacts was more effort than I found worth it on a daily basis except for special circumstances. Also, with contacts I had to be mindful of late activities as the longer I wore contacts in a day, the more bothersome they would become and of course I couldn't fall asleep wearing contacts.
As an additional benefit, my employer offers a discount on Lasik procedures to correct vision. With my health stabilizing once again and no scheduled medical procedures for the year, I decided this was the year to finally undergo Lasik.
With any type of procedure, my PTSD becomes triggered and I experience severe anxiety. I spoke with several individuals who previously underwent Lasik and each person reassured me that the procedure is not painful at all. I was informed that the eyes are numbed with drops and the laser surgery itself takes mere seconds.
After completing a qualifying exam, I scheduled my Lasik. I was provided a single Valium to take upon the completion of paperwork the day of the surgery to help ease my nerves. The last time I took Valium for a procedure was in 2009 when I underwent a 6 month follow up procedure to ensure that the Essure procedure I had underwent was successful. At this time, my anxiety was so severe that even with two doses of Valium, my nerves wouldn't allow the Valium to take effect until after the procedure was completed. I feared this would be the case again now but I repeatedly reminded myself that Lasik would be a painless procedure.
Lasik is completed with the use of a laser to reshape the cornea after a flap of corneal tissue is created. Lasik is an outpatient surgery that takes about 15 minutes to complete. It is such a quick procedure, that Lasik centers are able to schedule several patients in a short amount of time. There are risks to any procedure that can be serious and should be thoroughly discussed with the surgeon.
After completing paperwork, I was directed to a waiting area to join other patients awaiting eye surgery. When it was my turn, I entered the room with my toy kitty that I take with me to medical procedures for added comfort. The surgeon joked with me and notified me that they actually keep a stuffed toy in the operating room for patients to hold on to if they so wish. I was provided a blanket for extra comfort and situated myself upon the operating table. A nurse stood next to me the entire time and walked me through every step of the surgery. She notified me that an instrument would be used to create a flap in my cornea and she turned on the instrument so that I could hear what it sounded like so that I wouldn't be caught off guard. This particular instrument sounded like a drill used by a dentist. It was a terrifying sound when considering that this would be used on my eyes. Drops were inserted in my eyes to numb my eyes. Tape was used to pull my eyelids back to open my eyelids enough for an eye speculum to be inserted to keep my eyelids open. I had no ability to close my eyelids even if I had tried. This was not painful at all although it sounds as though it might. My eye was cleaned with a swab and I was told that a device would be placed on my eye to create suction, I would notice some pressure but no pain. This device was placed on my eye and pushed down - I felt the pressure, but no real pain. This suction ring stabilizes the eye and lifts and flattens the cornea. She told the surgeon it was "building, building, stabilized" and the pressure stopped as the suction was completed. The nurse notified me the drill sound would be starting. Even with this alert, the drill sound startled me and I couldn't help but slightly move my head backwards more into the table. I couldn't see the drill or anything unusual, I could just hear it. I didn't feel anything...the sound was just unnerving as it sounds as though I should see and feel something, but I didn't. My vision remained clear until the surgeon did a swiping motion to move the cornea flap and my vision became extremely blurry and hazy. I was told to stare at a green light that was previously concentrated but now was a blur. I stared at this light for a few seconds, maybe 5 seconds, and then the flap was placed back in the correct position and my blurry vision returned to normal. Several drops of antibiotics and anti-inflammatory eyedrops were placed in my eye. It was time for the next eye and the same procedure was completed. And it was over. During the procedure, in order to calm myself I had to repeatedly remind myself that I wasn't experiencing any pain, this would be over soon, and to think of it as looking through a camera - not through my actual eye itself.
I was taken to another room and another doctor examined my eyes to ensure the cornea flaps had sealed and my eyes looked appropriate. As I waited for the doctor to start his exam, I noticed that I could clearly see letters on the opposite wall that I wouldn't have been able to clearly see previously. The doctor reviewed the instructions for prescription eyedrops for the week and all the dos and don'ts to follow and answer any remaining questions I had. I was provided ice packs, sunglasses, and three boxes of preservative free eyedrops for moisture and told to try to sleep for 4-5 hours and to keep my eyes closed for that period.
The numbing drops were starting to wear off on the ride home. Even with the sunglasses, I was finding any amount of light to be extremely painful upon my closed eyes. My eyes were beginning to feel dry, like sandpaper but I couldn't rub my eyes as this would cause damage to my eyes and risk regression of my improved vision. Once home, I tried to sleep but the Valium had worn off and I was so bothered by the sandpaper feel that I was barely able to sleep. I could barely open my eyes, the sandpaper sensation was so intense. When I did manage to slightly open my eyes, they would immediately tear up and tears streamed down my face. This actually provided some comfort as it moistened my eyes. I had set my alarm to insert the eyedrops as directed and found this extremely challenging on account of the difficulty to open my eyes enough to insert drops. I began to question why I had decided to undergo Lasik. If I could just sleep until this passed, I would have been much more comfortable. I was only able to doze for brief periods through the sandpaper sensation. Finally, over the course of time the sensation began to lessen and my comfort increased. After about 5 hours, the sensation had ceased and I was able to comfortably open my eyes and clearly see things that were previously blurry to me.
I was instructed to use the prescription eyedrops four times a day for a week and to use preservative free artificial tears every 1-2 hours for the next two weeks. I wasn't allowed to wear make up for a week and no eye make up for two weeks. Aerobic exercise was prohibited for a few weeks. I was advised to not rub my eyes ever again, to take Omega 3 fatty acids, drink 5 glasses a water a day to help protect my vision from regression.
Two weeks later and my vision is 20/15! Extremely close objects in front of my eyes are blurry whereas they weren't previously but it isn't enough to interfere with anything and I normally don't have anything extremely close to my eyes anyway. I'm told that my vision should continue to improve over the next 6 months as my eyes continue to heal. I haven't driven at night yet to know how my vision is affected by lights at night. I'm told to expect halos and glare at night from lights for a few months although every individual is different. A second follow up occurs after 2-3 months and a final follow up around 6 months.
I'm pleased with my present outcome of the Lasik eye surgery. At times, I'm not certain if I would elect to undergo Lasik again but I am enjoying no longer requiring eyeglasses or contacts and the ability to see long distance for a change.
Labels:
Procedures
 This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
Monday, January 8, 2018
Reviewing Young Living Essential Oils for GI Symptoms
Disclaimer: I have been given this product as part of a product review. Although the product was a gift, all opinions in this review remain my own and I was in no way influenced by the company.
With worsening GI symptoms of chronic bloating, abdominal pain, and nausea interfering with my quality of life and a lack of improvement with prescription medications, I decided to try Essential Oils to address my bothersome symptoms. Rachel, with Young Living Essential Oil, provided a sample for my symptoms.
I was skeptical of oils being able to help with my pain but with desperate times come desperate measures. Prescription medications were no longer managing my bloating, pain, and nausea to my satisfaction. However, I have used peppermint oil by itself before to ease my nausea. Oils can be applied topically and some may be ingested.
It's recommended to apply peppermint oil to the soles of the feet or on the abdomen. I previously
applied peppermint oil to both locations without any improvement to my nausea. However, as long as I was able to smell the peppermint oil my nausea was subdued. I decided to resume using peppermint oil by rubbing a couple drops under my nose and reapplying as needed. In the case of severe nausea when I've been unable to tolerate visual movements such as watching tv or even reading, I applied a large amount to my abdomen and a small amount under my nose with noticeable improvements to my nausea. With the nausea relief provided by the peppermint oil, I decided to give DiGize Essential Oil a try for my bloating and abdominal pain.
applied peppermint oil to both locations without any improvement to my nausea. However, as long as I was able to smell the peppermint oil my nausea was subdued. I decided to resume using peppermint oil by rubbing a couple drops under my nose and reapplying as needed. In the case of severe nausea when I've been unable to tolerate visual movements such as watching tv or even reading, I applied a large amount to my abdomen and a small amount under my nose with noticeable improvements to my nausea. With the nausea relief provided by the peppermint oil, I decided to give DiGize Essential Oil a try for my bloating and abdominal pain.
DiGize is a blend of oils that can be used topically or ingested as a dietary supplement and includes the following oils all used to address heartburn, bloating, nausea, stomach cramps:
I'm not comfortable with ingesting oils as a dietary supplement, although I believe the oil would be more effective ingested versus topical application. Due to this discomfort, I was instructed to apply 1-3 drops to my abdomen or the soles of my feet and I could reapply as needed.
The first time I used the DiGize was the second consecutive day I had been feeling well after two completely miserable days due to my chronic bloating, pain, and nausea. For these two days, I had been tolerating food decently well and even was able to enjoy a night out with friends. However, this first night to try DiGize was after I decided to eat a snack without any of my other medications. Although my bloating and pain were not severe after this snack - they were bothersome.
I have a midline scar and scars on each side of my midline from my previous ostomy stomas. Due to my scars being a thicker skin, I decided to apply about three drops of oil in between my scars on both sides of my midline scar equaling about six drops. I waited approximately 10 minutes with some improvement to my bloating and pain before applying a second dosing of the same amount to the same spots. After about another ten minutes, I noticed a greater improvement to my symptoms to my satisfaction.
I started using the peppermint oil regularly to combat my chronic nausea and saved the Digize for when my stomach became bothersome or remained bothersome even with the medications I take with meals. I've found that my nausea is no longer a daily nuisance anymore after more than two years of enduring it on a daily basis. The combination of my meal medications with the Digize has been a promising combination as the Digize provided the final push my symptoms needed to significantly reduce in severity.
If you're interested in trying any of the oils, I encourage you to contact Rachel for guidance on recommended oils specific to your bothersome symptoms. You may also find her on Facebook or purchase oils here with international shipping available.
I started using the peppermint oil regularly to combat my chronic nausea and saved the Digize for when my stomach became bothersome or remained bothersome even with the medications I take with meals. I've found that my nausea is no longer a daily nuisance anymore after more than two years of enduring it on a daily basis. The combination of my meal medications with the Digize has been a promising combination as the Digize provided the final push my symptoms needed to significantly reduce in severity.
If you're interested in trying any of the oils, I encourage you to contact Rachel for guidance on recommended oils specific to your bothersome symptoms. You may also find her on Facebook or purchase oils here with international shipping available.
 This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
This is my life with Familial Adenomatous Polyposis and Short Bowel Syndrome.
I was diagnosed with FAP as a child, underwent total colectomy at age 9. I experienced life threatening complications resulting in 4 more surgeries that year and developing medical PTSD. I had an ileostomy for 6 years before having it reversed into a straight pull-thru that also resulted in life threatening complications requiring an additional surgery the following year. In 2021, I required my 8th surgery to remove my gall bladder due to gall stones and FAP. This surgery exacerbated my, at the time undiagnosed, Abdominal Migraine which is now being treated.
Subscribe to:
Posts (Atom)