I attended a seminar about
Probiotics, Food, and the Immune System presented by the
Institute for Natural Resources. This is just one of the many topics INR Seminars provides for healthcare professionals. The material is written by an expert and then presented by various educators. This particular seminar's syllabus was written by Dr. Nikita Katz, M.D., Ph.D. and was presented by Dr. Laura Pawlak, Ph.D., R.D. emerita.
This 6 hour seminar covered an intense amount of information about how the immune system works and is affected by foods and probiotics (healthy bacteria) with a specific focus on pro-inflammatory and anti-inflammatory influences. I will not be going into as much detail as the seminar provided.

Dr. Pawlak began by explaining that in the big picture there is a reciprocal interaction between food and environment on the immune system and on an individual's microbiota that then may affect the brain. The particular focus was placed upon the effects of pro or anti inflammatory properties that may protect or hinder the body as genes become expressed and diseases occur. Food and the probiotics that are found within our food or through medicinal supplements impact these protective or harmful factors and how our immune system functions.
Probiotics are commonly recommended for individuals with digestive disorders or diseases to help maintain a healthy gut flora that is easily disrupted by digestive disease. Probiotics are also recommended to be taken following the use of antibiotics in order to help replenish the good gut bacteria that is stripped away by antibiotics. To understand the importance of probiotics, it helps to have an awareness of the effects of microbiota on the body and interaction with the immune system.
Our immune system is made to protect us against threats that are not considered "self". Typically, immune responses are elicited from viruses, bacteria, and parasites that cause infectious diseases but can also be prompted by our own cells that look different than expected, such as cancerous cells. Immune responses are aggressive and must be controlled as the immune system has the capability to kill the identified organism, or person, itself.
The human microbiota is a combination of microorganisms that includes bacteria, fungi and archaea. Some microbiota found within humans are beneficial to the body whereas others may be harmful. There is a delicate balance required for human microbiota and its essential role for a healthy immune system and various neurobiological functions.
The Human Microbiome Project found that there are thousands of bacterial types found within an individual and different body sites have their own distinctive bacterial communities. The specific bacterial makeup for a given body site varies from person to person by type and abundance. Due to each part of the body having a different microbial arrangement, different probiotics will target different areas. Not every probiotic will be helpful to every part therefore this needs consideration when selecting food and medications specifically for their probiotic benefits.
It's estimated that 500 to 1,000 species of bacteria live in the human gut. Gut flora has the largest numbers of bacteria and the greatest number of bacteria species in comparison to other parts of the body. These gut bacteria are predominately Firmicutes and Bacteroidetes but others present also include Proteobacteria, Verrumicrobia, Actinobacteria, Fusobacteria, and Cyanobacteria. The gut flora is established within one to two years after birth which is enough time to allow for the intestinal epithelium and mucosal barrier to support the gut flora and provide a barrier to pathogenic organisms. Probiotics help protect the mucosal surface barrier from inflammation. When this barrier weakens due to inflammation, resistance to malignancy is reduced and cancer and inflammatory disorders may occur. With weakening of the barriers, we risk microbiota leakage or absorption in between cells where we do not want absorption. The brain receives every nutrient introduced to the body and probiotics activate the vagus nerve that reaches from the abdomen to the brain. The blood brain barrier allows nutrients to reach the brain while limiting harmful substances reaching the brain. However, with weakening of the barriers due to inflammation, harmful substances may pass through the blood brain barrier.
Depending on our food choices, certain foods can help keep good microbiota alive and bad microbiota down and vica versa. Fiber and oils promote the good whereas sugar and fats promote the bad. You may notice this when constipation occurs as bad microbiota likes constipation. Once the diet falls apart, so does the immune system. Diet also influences the type of microbiota present. A healthy diet promotes healthy microbioata whereas unhealthy foods promote harmful microbiota. Nutrients are vital for efficiency of the immune system.
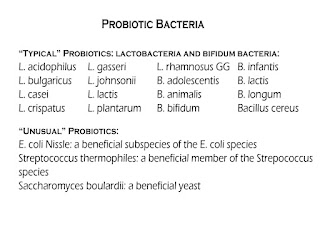
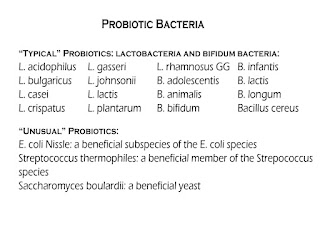 |
| Typical and Unusual Types of Probiotic Bacteria for Healthy Gut Flora |
Foods that naturally contain probiotic bacteria include:
Fermented cruciferous vegetables, fermented root vegetables and legumes, and sour milk products such as:
- Yogurt, recommended to be plain yogurt with no added sugar and labeled with live and active cultures. To sweeten, add fruit. Avoid adding sugar, artificial sweetners, or honey
- Kefir
- Icelandic skyr
- Swedish filmjolk
- Buttermilk
- Acidophilus milk
- Crème fraiche etc.
Non-dairy foods:
- Kombucha
- Kimchi
- Sauerkraut
- Green olives
- Tempeh
- Szechwan vegetable
- Indian pickle
- Mixed pickle
Another method for delivery of healthy probiotic bacteria is the Fecal Microbiota Transplant (Stool Transplant) to aid in restoring healthy colonic microflora by introducing healthy bacterial flora from the stool of a healthy donor by means of an enema, orogastric tube, or an oral capsule. This has been shown to be effective for C. Diff infections and is being used experimentally for treatment of other GI diseases including colitis, constipation, IBS and neurological conditions.
For the growth and activity of probiotics, prebiotics are necessary. Prebiotics are typically non-digestible fiber compounds in foods such as chicory root, Jerusalem artichoke, dandelion greens, garlic, leeks, asparagus, wheat bran, whole wheat flour, and bananas. There is not a broad consensus on an ideal daily serving of prebiotics but recommendations typically range from 4 to 8 grams for general digestive health and up to 15 grams for an individual with a digestive disorder.
There are diseases and syndromes linked to bacterial imbalance and immune dysfunction. These imbalances can occur in various parts of the body where the microbiota has deranged. In such instances, the normally dominating bacteria species become underrepresented and the normally outcompeted or contained species increase to fill the void. This dysbiosis, or microbial imbalance, is most commonly reported as a condition of the GI tract, particularly when there is an overgrowth in the small intestine of bacteria or fungi. This has been reported to be associated with illnesses such as periodontal disease, IBD, chronic fatigue syndrome, cancer, and colitis. It may be important to note that patients treated with PPIs to reduce stomach acid tend to have a higher frequency of small intestine bacterial overgrowth.
Microbes within a tumor can affect cancer growth and spread. Microbes and microbiota affect cancer formation by altering the balance of tumor cell life and death, immune system function regulation, and influencing the metabolism of foods and pharmaceuticals.
Mucosal surface barriers within the body require rapid repair, once these barriers are breached then microbes can elicit pro-inflammatory or immunosuppressive programs thereby allowing cancer and inflammatory disorders to occur. Probiotics can help protect the mucosal surface barriers against inflammation.
Inflammation is a biological response of body tissues to harmful stimuli and a protective response. Inflammation functions to eliminate the initial cause of cell injury, remove necrotic cells and tissues damaged from the original insult and start tissue repair. The typical signs of inflammation include heat, pain, redness, swelling, and loss of function. Inflammation may be acute or chronic. Prolonged inflammation can lead to a progressive shift in the type of cells present at the inflamed area. Inflammation can cause disease related genes to be expressed and is linked to most chronic diseases including arthritis, cancers, cardiovascular diseases, IBD, and diabetes.
Of the dietary components tested thus far on the Dietary Inflammatory Index (DII) for pro-inflammatory and anti-inflammatory properties, the top anti-inflammatory components include Turmeric, Omega 3 Fatty Acids, Fiber, Genisten (protein found in soybeans), Tea - the leaves are best, Alcohol - wine berries, and Magnesium. Turmeric should be taken with fresh ground black pepper in 10 parts turmeric to 1 part pepper for optimal absorption. the DII has a long way to go still as only a handful of dietary components have been tested for their pro and anti inflammatory properties.
When thinking of maintaining a healthy immune system, we must take in consideration not only the foods we ingest but also our exposure to environmental factors. With the advance of technology, we are now exposed to chemical compounds that were not naturally occurring on the planet previously and we are now exposed to chemicals normally hidden within the ground that are now exposed through mining and manufacturing. Heavy metals exposure causes significant alterations to the immune system by increasing the body's pro-inflammatory and decreasing anti-inflammatory responses. Air pollutants, pesticides, phthalates, PCBs, and perfluoralkyl substances exposure are also associated with medical conditions.
To help reduce one's susceptibility to immune dysfunction associated with such environmental influences, it's recommended to choose phthalate free personal care products, fresh foods rather than processed foods, and reduce exposure to pesticides, heavy metals, and air pollutants as much as possible.
To help lower inflammation and maintain a healthy microbiota balance, it is recommended to eat healthy, fresh foods, ingest probiotics, obtain adequate sleep , exercise regularly, and reduce stress. Exercise secretes proteins that are anti-inflammatory and remaining in the stressful fight or flight crisis response mode increases inflammation.